What is Liver Cancer?
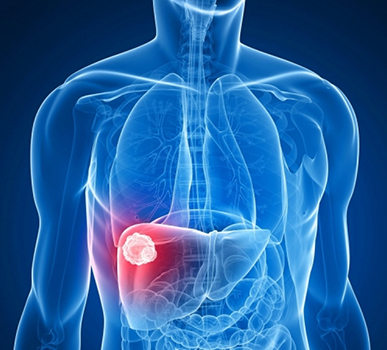
Liver cancer, also known as hepatocellular cancer, is a cancer that originates in the liver itself. Liver cancer occurs when abnormal cells within the liver grow in an uncontrolled way. A tumor can be cancerous or benign. A cancerous tumor is malignant, meaning it can grow and spread to other parts of the body.
What causes liver cancer?
Liver cancer happens when liver cells develop changes (mutations) in their DNA. A cell's DNA is the material that provides instructions for every chemical process in your body. DNA mutations cause changes in these instructions. One result is that cells may begin to grow out of control and eventually form a tumor - a mass of cancerous cells.
CAN-C: We provide high-standard liver cancer treatment in Bangalore.
Here, you will find information about signs and symptoms, causes and risk factors, types, diagnosis, staging and prevention about liver cancer.
Most people don't have signs and symptoms in the early stages of primary liver cancer. Some of the most common symptoms of liver cancer are:
Weight loss (without trying)
Loss of appetite
Feeling very full after a small meal
Nausea or vomiting
An enlarged liver, felt as fullness under the ribs on the right side
An enlarged spleen, felt as fullness under the ribs on the left side
Pain in the abdomen (belly) or near the right shoulder blade
Swelling or fluid build-up in the abdomen (belly)
Itching, General weakness and fatigue
Yellowing of the skin and eyes (jaundice)
White, chalky stools
CAN-C is a cancer centre specially designed for patients receiving liver cancer treatment in Bangalore.
Factors that increase the risk of liver cancer include:
Excessive alcohol consumption: Consuming more than a moderate amount of alcohol daily over many years can lead to irreversible liver damage and increase your risk of liver cancer.
Tobacco use: Smoking increases the risk of liver cancer.
Obesity: Being obese (very overweight) increases the risk of developing liver cancer. This is probably because it can result in fatty liver disease and cirrhosis.
Type 2 diabetes: Type 2 diabetes has been linked with an increased risk of liver cancer, usually in patients who also have other risk factors such as heavy alcohol use and/or chronic viral hepatitis. This risk may also be increased because people with type 2 diabetes tend to be overweight or obese, which in turn can cause liver problems.
Cirrhosis: This progressive and irreversible condition causes scar tissue to form in your liver and increases your chances of developing liver cancer.
Chronic infection with HBV or HCV: Chronic infection with the hepatitis B virus (HBV) or hepatitis C virus (HCV) increases your risk of liver cancer.
Exposure to aflatoxins: Aflatoxins are poisons produced by molds that grow on crops that are stored poorly. Crops, such as grains and nuts, can become contaminated with aflatoxins, which can end up in foods made of these products.
Vinyl chloride and thorium dioxide (Thorotrast): Exposure to these chemicals raises the risk of angiosarcoma of the liver. It also increases the risk of developing cholangiocarcinoma and hepatocellular cancer.
Anabolic steroids: Long-term anabolic steroid (used by some athletes to increase their strength and muscle mass) use can slightly increase the risk of hepatocellular cancer.
Inherited metabolic diseases: Certain inherited metabolic diseases can lead to cirrhosis.
The different types of cells in the liver can form several types of malignant (cancerous) and benign (non-cancerous) tumors. These tumors have different causes, are treated differently, and have a different prognosis (outlook).
Primary liver cancer:
A cancer that starts in the liver is called primary liver cancer. There is more than one kind of primary liver cancer.
Hepatocellular carcinoma (HCC): This is the most common form of liver cancer in adults. Hepatocellular cancers can have different growth patterns: Some begin as a single tumor that grows larger. Only late in the disease does it spread to other parts of the liver and a second type seems to start as many small cancer nodules throughout the liver, not just a single tumor.
Intrahepatic cholangiocarcinoma (bile duct cancer): About 10% to 20% of cancers that start in the liver are intrahepatic cholangiocarcinomas. These cancers start in the cells that line the small bile ducts (tubes that carry bile to the gallbladder) within the liver. Most cholangiocarcinomas, however, actually start in the bile ducts outside the liver.
Angiosarcoma and hemangiosarcoma: These are rare cancers that begin in cells lining the blood vessels of the liver. These tumors grow quickly and are usually too widespread to be removed surgically by the time they are found.
Hepatoblastoma: This is a very rare kind of cancer that develops in children, usually in those younger than 4 years old. The cells of hepatoblastoma are similar to fetal liver cells.
Secondary liver cancer (metastatic liver cancer):
Most of the time when cancer is found in the liver it did not start there but has spread (metastasized) from somewhere else in the body, such as the pancreas, colon, stomach, breast, or lung. Because this cancer has spread from its original (primary) site, it is called a secondary liver cancer. These tumors are named and treated based on their primary site (where they started). For example, cancer that started in the lung and spread to the liver is called lung cancer with spread to the liver, not liver cancer. It is also treated as lung cancer.
Some liver cancers can be found by testing people at high risk who don't have symptoms (screening), but most liver cancers are found because they are causing symptoms. If you have possible signs or symptoms of liver cancer, see your doctor, who will examine you and may order some tests.
Medical history and physical exam: Your doctor will also examine you to look for signs of liver cancer and other health problems, probably paying special attention to your abdomen and checking your skin and the whites of your eyes looking for jaundice (a yellowish color).
Imaging tests: Imaging tests use x-rays, magnetic fields, or sound waves to create pictures of the inside of your body. Imaging tests maybe done for a number of reasons both before and after a diagnosis of liver cancer.
Ultrasound: Ultrasound is the test used to look at the liver. It uses sound waves to create an image on a computer screen. This test can show tumors growing in the liver, which then can be tested for cancer, if needed.
Computed tomography (CT): The CT scan is an x-ray test that makes detailed images of your body. A CT scan of the abdomen can help find many types of liver tumors. It can give specific information about the size, shape, and location of any tumors in the liver or elsewhere in the abdomen, as well as nearby blood vessels.
Magnetic resonance imaging (MRI): Like CT scans, MRI scans provide detailed images of soft tissues in the body. But MRI scans use radio waves and strong magnets instead of x-rays. MRI scans can be very helpful in looking at liver tumors. They can also be used to look at blood vessels in and around the liver to see any blockages, and can help show if liver cancer has spread to other parts of the body.
Angiography: An angiogram is an x-ray test that looks at blood vessels. Contrast medium, or dye, is injected into an artery to outline blood vessels while x-ray images are taken.
Biopsy: A biopsy is the removal of a sample of tissue to see if it is cancer. Sometimes, the only way to be sure that liver cancer is present is to take a biopsy and look at it in the pathology lab.
CAN-C provides best liver cancer treatment in Bangalore.
Staging is a way of describing where the cancer is located, if or where it has spread, and whether it is affecting other parts of the body. Staging a cancer helps determine the prognosis of the disease, which is the chance of recovery, and the types of treatment that are most appropriate. In general, only early-stage liver cancer can be cured.
How is the stage determined?
There are several staging systems for liver cancer and the most often used is the TNM system, which is based on 3 key pieces of information:
The extent (size) of the tumor (T): How large has the cancer grown? Is there more than one tumor in the liver? Has the cancer reached nearby structures like the veins in the liver?
The spread to nearby lymph nodes (N): Has the cancer spread to nearby lymph nodes?
The spread (metastasis) to distant sites (M): Has the cancer spread to distant lymph nodes or distant organs such as the bones or lungs?
Once a person's T, N, and M categories have been determined, this information is combined in a process called stage grouping to assign an overall stage.
Whatever your cancer stage, we at CAN-C in Bangalore provide personalized treatment plan for liver cancer.
Liver cancers could be prevented by reducing exposure to known risk factors:
Limit alcohol consumption: Drinking alcohol can lead to cirrhosis, which in turn, can lead to liver cancer. Not drinking alcohol or drinking in moderation could help prevent liver cancer.
Stop using tobacco: Since smoking also increases the risk of liver cancer, not smoking will also prevent some of these cancers. If you smoke, quitting will help lower your risk of this cancer, as well as many other cancers and life-threatening diseases.
Get to and stay at a healthy weight: If your current weight is healthy, work to maintain it by choosing a healthy diet and exercising most days of the week. If you need to lose weight, reduce the number of calories you eat each day and increase the amount of exercise you do.
Avoid and treat hepatitis B and C infections: The most significant risk factor for liver cancer is chronic infection with hepatitis B virus (HBV) and hepatitis C virus (HCV). These viruses can spread from person to person through sharing contaminated needles (such as in drug use) through unprotected sex, and through childbirth.
Limit exposure to cancer-causing chemicals: Reduce exposure to cancer-causing substances such as aflatoxins.
"CAN-C: Developed a reputation for liver cancer treatment in Bangalore."
Make An Appointment Today
How Liver Cancer is treated?
The treatment for liver cancer depends on: where your cancer is, the size of the cancer and whether it has spread (the stage), the type of cancer, how well your liver is working, your general health and level of fitness. Treatment options include destroying or slowing the growth of cancer. The most common treatments for secondary cancer in the liver are listed below. Often a combination of therapies is used.
The best option to cure liver cancer is with either surgical resection (removal of the tumor with surgery) or a liver transplant. If all cancer in the liver is completely removed, you will have the best outlook. Small liver cancers may also be cured with other types of treatment such as ablation or radiation.
1. Partial hepatectomy
Partial hepatectomy is surgery to remove part of the liver. Only people with good liver function who are healthy enough for surgery and who have a single tumor that has not grown into blood vessels can have this operation. Imaging tests, such as CT or MRI with angiography are done first to see if the cancer can be removed completely.
People with cirrhosis are typically eligible for surgery if there is only one tumor (that has not grown into blood vessels) and they will still have a reasonable amount (at least 30%) of liver function left once the tumor is removed.
2. Liver transplant
When it is available, a liver transplant may be the best option for some people with liver cancer. Liver transplants can be an option for those with tumors that cannot be removed with surgery, either because of the location of the tumors or because the liver has too much disease for the patient to tolerate removing part of it. In general, a transplant is used to treat patients with small tumors that have not grown into nearby blood vessels. It can also rarely be an option for patients with resectable cancers (cancers that can be removed completely).
We pride ourselves in being known for top-quality liver cancer treatment in Bangalore.
Radiation therapy uses high-energy rays (or particles) to kill cancer cells. It may not be a good option for some patients whose liver has been greatly damaged by diseases such as hepatitis or cirrhosis.
Radiation can be helpful in treating:
1. Liver cancer that cannot be removed by surgery
2. Liver cancer that cannot be treated with ablation or embolization or did not respond well to those treatments
3. Liver cancer that has spread to other areas such as the brain or bones
4. People with pain because of large liver cancers
5. People with a tumor thrombus (a collection of liver cancer cells) blocking the portal vein.
How is radiation therapy given?
1. External beam radiation therapy (EBRT) focuses radiation from a source outside of the body on the cancer. Getting radiation therapy is much like getting an x-ray, but the radiation is stronger. The procedure itself is painless.
2. Although liver cancer cells are sensitive to radiation, much care is taken when planning the treatment to avoid damaging normal liver tissue as much as possible. Newer radiation techniques, such as stereotactic body radiation therapy (SBRT), help doctors target liver tumors while reducing the radiation to nearby healthy tissues. This makes it more effective and reduces side effects. SBRT allows treatment to be completed in a short-time compared to EBRT. It uses very focused beams of high-dose radiation given on one or a few days. Beams are aimed at the tumor from many different angles.
3. Radioembolization: Tumors in the liver can be treated by injecting small radioactive beads into the hepatic artery. The beads then lodge in the liver near the tumor and give off small amounts of radiation that travel only a short distance.
Chemotherapy (chemo) is treatment with drugs to destroy cancer cells. Chemo may be an option for people whose liver cancer cannot be treated with surgery, has not responded to local therapies such as ablation or embolization, or when targeted therapy is no longer helpful.
Recent advances have shown that a combination of drugs may be more helpful than using just a single chemo drug. But even these combinations of drugs shrink only a small number of tumors, and the responses often do not last long. The most common chemotherapy drugs for treating liver cancer include:
Gemcitabine (Gemzar), Oxaliplatin (Eloxatin), Cisplatin, Doxorubicin (pegylated liposomal doxorubicin), 5-fluorouracil (5-FU), Capecitabine (Xeloda), Mitoxantrone (Novantrone)
Sometimes, combinations of 2 or 3 of these drugs are used. GEMOX (gemcitabine plus oxaliplatin) is one option for people who are fairly healthy and may tolerate more than one drug. 5-FU based chemotherapy, for example with FOLFOX (5-FU, oxaliplatin and leucovorin), is another option for people with bad liver disease.
You can get chemotherapy in different ways.
1. Systemic chemotherapy: Drugs are injected right into a vein (IV) or taken by mouth. These drugs enter the bloodstream and reach almost all areas of the body, possibly making this treatment useful for cancers that have spread to other parts of the body.
2. Regional chemotherapy: Drugs are put right into an artery that leads to the part of the body with the tumor. This focuses the chemo on the cancer cells in that area. It reduces side effects by limiting the amount of drug reaching the rest of the body. Hepatic artery infusion, or chemo given directly into the hepatic artery, is regional chemotherapy that can be used for liver cancer.
3. Hepatic artery infusion: Putting chemo drugs directly into the hepatic artery at a constant rate to see if it might be more effective than systemic chemo. This technique is known as hepatic artery infusion (HAI). It is slightly different from chemoembolization because surgery is needed to put an infusion pump under the skin of the abdomen (belly).
Targeted drugs work differently from standard chemotherapy drugs. Like chemotherapy, these drugs enter the bloodstream and reach almost all areas of the body, which makes them potentially useful against cancers that have spread to distant parts of the body. Because standard chemo has not been effective in most patients with liver cancer, doctors have been looking at targeted therapies more.
1. Tyrosine kinase inhibitors: Kinases are proteins on or near the surface of a cell that carry important signals to the cell’s control center. The targeted drugs (called tyrosine kinase inhibitors) block several kinase proteins that help tumor cells grow or help tumors form new blood vessels to feed itself. Blocking these proteins can help stop the growth of cancer cells.
2. Sorafenib (Nexavar) and lenvatinib (Lenvima): These drugs can be used to treat liver cancer if it cannot be treated by surgery or if it has spread to other organs. Sorafenib may work better in people with liver cancer caused by hepatitis C.
3. Regorafenib (Stivarga) and cabozantinib (Cabometyx): These drugs can be used to treat liver cancer if sorafenib is no longer helpful.
4. Ramucirumab (Cyramza): Ramucirumab is used to treat advanced liver cancer if sorafenib stops working. It works mainly by keeping the cancer from making more blood vessels.
CAN-C: The centre of excellence that cater to each and every patient's needs by providing technologically advanced liver cancer treatment in Bangalore.
Immunotherapy is the use of medicines that help a person's own immune system find and destroy cancer cells. It can be used to treat some people with liver cancer.
Immune checkpoint inhibitors
An important part of the immune system is its ability to keep itself from attacking normal cells in the body. To do this, it uses "checkpoints" - proteins on immune cells that need to be turned on (or off) to start an immune response. Cancer cells sometimes use these checkpoints to avoid being attacked by the immune system. But newer drugs that target these checkpoints hold a lot of promise as cancer treatments.
Pembrolizumab (Keytruda) and nivolumab (Opdivo) are drugs that target PD-1, a protein on immune system cells called T cells that normally helps keep these cells from attacking other cells in the body. By blocking PD-1, these drugs boost the immune response against cancer cells. This can shrink some tumors or slow their growth.
These drugs can be used in people with liver cancer who have previously been treated with the targeted drug sorafenib (Nexavar). These drugs are given as an intravenous (IV) infusion.
In Bangalore, we are recognized for offering personalized liver cancer treatment options designed to meet your needs and improve your quality of life.
Our Doctors
Dr. Dinesh M G
Specialty: Surgical Oncologist & Laparoscopic Oncosurgeon
Dr. Dinesh M G, is an efficient surgeon specialized in oncology committed to the care and improvement of quality of life of cancer patients. His exceptional surgical skills, teamwork and knowledge are laudable. He is skilled in performing various minimal access oncologic surgeries and has mastered complex open surgeries in the field of oncology.
Completing MBBS from KIMS, Bangalore followed by MS - General Surgery from JJM Medical College, Davangere and M. Ch - Surgical Oncology from Kidwai Memorial Institute of Oncology, he has a Fellowship in Minimal Access Oncology from Basavatarakam Indo American Cancer Institute.

