What Is Penile Cancer?
Penile cancer, or cancer of the penis, is when cells grow out of control on or in a man's penis. It often starts in skin cells and can work its way inside. It occurs when normally healthy cells in the penis become cancerous and begin to grow out of control, forming a tumor.
CAN-C: Specialty centre for penile cancer treatment in Bangalore.
Here, you will find information about signs and symptoms, causes and risk factors, types, diagnosis, staging and prevention about penile cancer.
Signs and symptoms do not always indicate the person has penile cancer. In fact, many are more likely to be caused by other conditions. Some of the symptoms of penile cancer are listed below:
Skin changes: The first sign of penile cancer is most often a change in the skin of the penis. This is most likely to be on the glans (tip) of the penis or on the foreskin (in uncircumcised men), but it can also be on the shaft. These changes may include:
a. An area of skin becoming thicker
b. Changes in the skin colour
c. A lump
d. An ulcer (sore) that might bleed
e. A reddish, velvety rash under the foreskin
f. Small, crusty bumps
g. Flat, bluish-brown growths
h. Smelly discharge (fluid) or bleeding under the foreskin.
Swelling: Swelling at the end of the penis, especially when the foreskin is constricted, is another possible sign of penile cancer.
We are recognized as a well-known cancer centre for penile cancer treatment (in Bangalore) with latest treatment options.
The exact cause of most penile cancers is not known, but the researches have found that it could be linked with a number of conditions.
A risk factor is anything that affects your chance of getting a disease like cancer. Different cancers have different risk factors. Some risk factors of penile cancer include:
Human papillomavirus (HPV) infection: Human papillomavirus (HPV) is a group of more than 150 related viruses. They are called papillomaviruses because some of them cause growths called papillomas (more commonly called warts). Other HPV types have been linked with certain cancers.
Not being circumcised: Circumcision removes all (or part) of the foreskin. This procedure is most often done in infants, but it can be done later in life, too. Men who were circumcised as children may have a much lower chance of getting penile cancer than those who were not.
Phimosis and smegma: Uncircumcised men with certain conditions are at higher risk for penile cancer.
a. Phimosis: In men who are not circumcised, the foreskin can sometimes become tight and difficult to retract. This is known as phimosis.
b. Smegma: Sometimes secretions can build up underneath an intact foreskin. If the area under the foreskin is not cleaned well, these secretions build up enough to become a thick, sometimes smelly substance called smegma.
Smoking and other tobacco use: Men who smoke and/or use other forms of tobacco are more likely to develop penile cancer. Tobacco users who have HPV infections have an even higher risk.
UV light treatment of psoriasis: Men who have a skin disease called psoriasis are sometimes treated with drugs called psoralens and then an ultraviolet A (UVA) light source. This is called PUVA therapy. Men who have had this treatment have been found to have a higher rate of penile cancer.
Age: The risk of penile cancer goes up with age.
AIDS: Men with AIDS have a higher risk of penile cancer. This higher risk seems to be linked to their weakened immune system, which is a result of this disease.
Each type of tissue in the penis contains several types of cells. Different types of penile cancer can start from these cells. The differences are important because they determine the seriousness of the cancer and the type of treatment needed.
Almost all penile cancers start in skin cells of the penis.
Squamous cell carcinoma: About 95% of penile cancers start in flat skin cells called squamous cells. Squamous cell carcinoma (also known as squamous cell cancer) can start anywhere on the penis. Most of these cancers start on the foreskin (in men who have not been circumcised) or on the glans. These tumors tend to grow slowly. If they are found at an early stage, they can usually be cured.
Verrucous carcinoma: A verrucous carcinoma growing on the penis is also known as Buschke-Lowenstein tumor. This is an uncommon form of squamous cell cancer that can start in the skin in many areas. This cancer looks a lot like a large genital wart. Verrucous carcinomas tend to grow slowly but can sometimes get very large. They can grow deep into nearby tissue, but they rarely spread to other parts of the body.
Carcinoma in situ (CIS): This is the earliest stage of squamous cell cancer of the penis. In this stage, the cancer cells are found only in the top layers of skin. They have not yet grown into the deeper tissues. Depending on where the CIS is on the penis, doctors may use other names for the disease.
a. CIS of the glans is sometimes called erythroplasia of Queyrat.
b. CIS on the shaft of the penis (or other parts of the genitals) is called Bowen disease.
Melanoma: Melanoma is a type of skin cancer that starts in melanocytes, the cells that make the brownish color in the skin that helps protect it from the sun. These cancers tend to grow and spread quickly. They're more dangerous than the more common basal and squamous cell types of skin cancer. Melanomas are most often found in sun-exposed skin, but rarely they occur in other places like the penis. Only a very small portion of penile cancers are melanomas.
Basal cell carcinoma: Basal cell carcinoma (also known as basal cell cancer) is another type of skin cancer that can develop on the penis. It makes up only a small portion of penile cancers. This type of cancer is slow-growing and rarely spreads to other parts of the body.
Adenocarcinoma (Paget disease of the penis): This very rare type of penile cancer can develop from sweat glands in the skin of the penis. It can be very hard to tell apart from carcinoma in situ (CIS) of the penis.
Sarcoma: A small number of penile cancers are sarcomas. These cancers develop from blood vessels, smooth muscle, or other connective tissue cells of the penis.
We are recognized as the leading cancer centre in Bangalore for penile cancer treatment.
Screening tests include:
Medical history and physical exam.
Biopsy: A biopsy is the only sure way to know if a change is penile cancer. There are many ways a biopsy can be done:
a. Incisional biopsy: For an incisional biopsy only a part of the changed area is removed.
b. Excisional biopsy: In an excisional biopsy, the entire lesion is removed. This type of biopsy is most often used if the lesion is small, such as a nodule (lump) or plaque (raised, flat area).
c. Lymph node biopsy: If the cancer has spread deep within the penis, nearby lymph nodes usually will need to be checked for cancer spread.
d. Fine needle aspiration (FNA): To do this type of biopsy, the doctor puts a thin, hollow needle right into the lymph node and uses a syringe to pull out cells and a few drops of fluid.
e. Surgical biopsy: In some cases, the lymph nodes are not checked with FNA, but instead surgery is done to remove one or more lymph nodes. These surgical lymph node biopsies, which include sentinel lymph node biopsy and lymphadenectomy, are described in Surgery for Penile Cancer.
Imaging: If the enlarged lymph node is deep inside your body and the doctor cannot feel it, imaging methods like x-rays, magnetic fields, or sound waves are used.
a. Ultrasound.
b. CT scans can be used to guide the needle into the node.
c. Chest x-ray: An x-ray might be done to see if the cancer has spread to the lungs.
Once the cancer is diagnosed, it is necessary to figure out if it has spread, and if so, how far, which is called staging. The stage of a cancer describes how much cancer is in the body. It helps determine how serious the cancer is and how best to treat it.
How is the stage determined?
The staging system most often used for penile cancer is the TNM system, which is based on 3 key pieces of information:
The extent of the main tumor (T): How far has the cancer grown into the penis, and has it reached nearby tissues or organs?
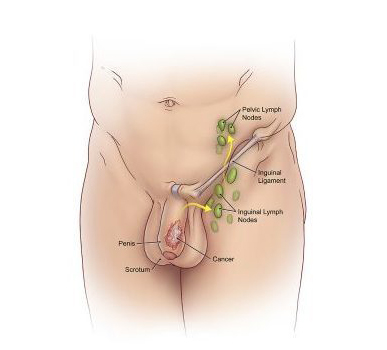
The spread to nearby lymph nodes (N): Has the cancer spread to nearby lymph nodes (in the groin and pelvic area)? If so, how many are affected?
The spread (metastasis) to distant sites (M): Has the cancer spread to distant parts of the body? (The most common sites of spread are distant lymph nodes or organs like the lung, liver, or bones.)
The large variations in penile cancer rates suggest that many penile cancers can be prevented. The best way to reduce the risk of penile cancer is to avoid known risk factors.
Genital hygiene: The most important factor in preventing penile cancer in uncircumcised men is good genital hygiene.
HPV infection: HPV is very common, so having sex with even one other person can put you at risk.
Tobacco use: Tobacco use also increases penile cancer risk, so not using any form of tobacco might lower the risk.
"CAN-C: The very best centre for penile cancer treatment in Bangalore."
Make An Appointment Today
How Penile Cancer is treated?
The treatment options for penile cancer are based mainly on the stage (extent) and grade of the cancer, but other factors can also be important. The most common treatment options for penile cancer are: Surgery, Chemotherapy, Radiotherapy, Targeted Therapy and Immunotherapy. We are dedicated to assure the best possible penile cancer treatment in Bangalore.
Surgery is the most common treatment for all stages of penile cancer. If the cancer is found when it is small without spreading the tumor can often be treated without having to remove part of the penis. Many different kinds of surgery are used to treat penile cancers. Penile-sparing techniques are used as often as possible.
a. Circumcision: If the cancer is only on the foreskin, circumcision can often cure the cancer.
b. Simple excision: In simple excision surgery, the tumor is cut out, along with some nearby normal skin.
c. In a wide local excision, the tumor is removed along with a large amount of normal tissue around it.
d. Mohs surgery (microscopically controlled surgery): This may be an option instead of wide local excision in select cases. Using the Mohs technique, the surgeon removes a layer of the skin that the tumor may have invaded and then checks the sample under a microscope right away. If it contains cancer, another layer is removed and examined. This process is repeated until the skin sample doesn't have cancer cells in it.
e. Glansectomy: If the tumor is small and only on the glans (the tip of the penis), part or all of it may be removed.
f. Partial or total penectomy: This operation removes part or all of the penis. It is the most common and best known way to treat penile cancer that has grown deeply inside the penis.
The operation is called a partial penectomy if only the end of the penis is removed (and some shaft remains). If not enough of the shaft can be saved for the man to urinate standing up without dribbling, a total penectomy will be done. The surgeon creates a new opening for urine to drain from the perineum, which is the area between the scrotum (sac for the testicles) and the anus. This is called a perineal urethrostomy. For very advanced tumors, sometimes the penis is removed along with the scrotum (and testicles). This operation is called emasculation.
g. Lymph node surgery: Men with cancer that has grown deep within the penis usually need to have some nearby lymph nodes in the groin removed so they can be checked for cancer spread.
Sentinel lymph node biopsy (SLNB): This operation can sometimes help the surgeon see if the groin lymph nodes contain cancer without having to remove all of them.
Inguinal lymphadenectomy (groin lymph node dissection): Many men with penile cancer have swollen groin lymph nodes when they're first diagnosed. These lymph nodes need to be removed if they contain cancer cells, but sometimes, the swelling is from infection or inflammation, not cancer.
h. Pelvic lymph node surgery: If cancer is found in 2 or more inguinal (groin) lymph nodes, pelvic lymph nodes will also be removed and checked.
CAN-C is one of the top cancer centres in Bangalore for penile cancer treatment.
Radiation therapy uses high-energy rays or particles to destroy cancer cells. It can be used to treat penile cancer in these ways:
a. It can be used to treat some smaller penile cancers instead of surgery.
b. If the cancer has spread to many lymph nodes, radiation may be used after surgery to remove the lymph nodes to try to reduce the risk the cancer will come back.
c. It can be used when surgery isn't an option.
d. Radiation can be used for advanced cancer to try to slow the growth of the cancer or to relieve symptoms it causes.
e. It can be given along with chemo before surgery to help shrink the tumor and make it easier to remove with less damage to the penis.
f. Men at high risk of cancer coming back in nearby lymph nodes might get radiation to those nodes to help lower this risk.
There are 2 main ways to get radiation therapy for penile cancer:
1. External beam radiation therapy: The most common way to get radiation therapy is from carefully focused beams of radiation aimed at the tumor from a machine. The treatment is a lot like getting an x-ray, but the radiation is much stronger.
2. Brachytherapy: For brachytherapy, a radioactive source is placed into or next to the penile tumor. The radiation travels only a short distance, so nearby healthy tissues do not get much radiation. There are 2 ways to get brachytherapy for penile cancer.
a. Interstitial radiation: In this method, hollow needles are first put into the penis in the operating room. Pre-drilled plastic templates lock onto both ends of the needles to hold them in place.
b. Plesiobrachytherapy: This type of brachytherapy puts the radiation source close to (but not into) the tumor. In this method, a plastic cylinder is fitted around the penis. This treatment can only work for tumors near the surface of the penis.
Chemotherapy (chemo) is the use of drugs to treat cancer. Two types of chemotherapy can be used in treating penile cancer:
a. Topical chemotherapy: Topical chemotherapy means that a cancer-killing drug is put right on the skin instead of taken as a pill or injected into a vein. The drug used most often to treat penile cancer this way is 5-fluorouracil (5-FU).
b. Systemic chemotherapy: Systemic chemo uses cancer-killing drugs that are injected into a vein or given by mouth. These drugs go through the bloodstream and reach cancer cells throughout the body. This treatment is most often used for penile cancers that have spread to lymph nodes or distant organs. Chemo might also be used to shrink tumors before surgery to make them easier to remove.
Some of the drugs used to treat penile cancer include: Cisplatin, Fluorouracil (5-FU), Paclitaxel (Taxol®), Ifosfamide (Ifex®), Mitomycin C, Capecitabine (Xeloda®).
Often, 2 or more of these drugs are used together to treat penile cancer that has spread to lymph nodes or other organs. Some common combinations include: Cisplatin plus 5-FU, TIP: paclitaxel (Taxol), ifosfamide, and cisplatin ("platinum").
In Bangalore, we at CAN-C are the renowned centre for penile cancer treatment.
Our Doctors
Dr. Dinesh M G
Specialty: Surgical Oncologist & Laparoscopic Oncosurgeon
Dr. Dinesh M G, is an efficient surgeon specialized in oncology committed to the care and improvement of quality of life of cancer patients. His exceptional surgical skills, teamwork and knowledge are laudable. He is skilled in performing various minimal access oncologic surgeries and has mastered complex open surgeries in the field of oncology.
Completing MBBS from KIMS, Bangalore followed by MS - General Surgery from JJM Medical College, Davangere and M. Ch - Surgical Oncology from Kidwai Memorial Institute of Oncology, he has a Fellowship in Minimal Access Oncology from Basavatarakam Indo American Cancer Institute.

