What is Skin Cancer?
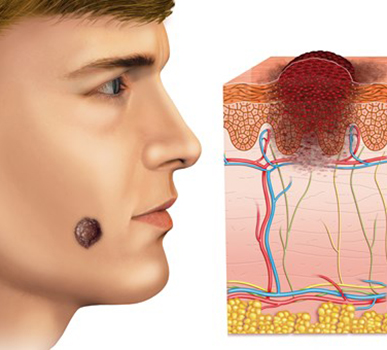
Skin cancer is a disease in which malignant (cancer) cells form in the tissues of the skin. Early detection of skin cancer gives you the greatest chance for successful skin cancer treatment. Skin cancer develops when one of the three types of cells that make up your skin reproduce abnormally. As they grow and divide without stopping, they can metastasize. This means they spread to other places in your body through your lymphatic system.
What Causes It?
Skin cancer is the out-of-control growth of abnormal cells in the epidermis, the outermost skin layer, caused by unrepaired DNA damage that triggers mutations. These mutations lead the skin cells to multiply rapidly and form malignant tumors. The main types of skin cancer are basal cell carcinoma (BCC), squamous cell carcinoma (SCC), melanoma and Merkel cell carcinoma (MCC).
In Bangalore, we provide best treatment for skin cancer with highest care.
Here, you will find information about signs and symptoms, causes and risk factors, types, diagnosis, staging and prevention about skin cancer.
Basal and squamous cell skin cancers are more common than melanomas, but they are usually very treatable. Symptoms are:
Flat, firm, pale or yellow areas, similar to a scarc
Raised reddish patches that might be itchy
Small, pink or red, translucent, shiny, pearly bumps, which might have blue, brown, or black areas
Pink growths with raised edges and a lower area in their center, which might contain abnormal blood vessels spreading out like the spokes of a wheel
Open sores (which may have oozing or crusted areas) that don't heal, or that heal and then come back
Wart-like growths
Rough or scaly red patches, which might crust or bleed
Raised growths or lumps, sometimes with a lower area in the center
Possible signs and symptoms of melanoma:
New spot on the skin or a spot that is changing in size, shape, or color.
A spot that looks different from all of the other spots on your skin (known as the ugly duckling sign).
The ABCDE rule is another guide to the usual signs of melanoma:
A is for Asymmetry: One half of a mole or birthmark does not match the other.
B is for Border: The edges are irregular, ragged, notched, or blurred.
C is for Color: The color is not the same all over and may include different shades of brown or black, or sometimes with patches of pink, red, white, or blue.
D is for Diameter: The spot is larger than 6 millimeters across (about ¼ inch - the size of a pencil eraser), although melanomas can sometimes be smaller than this.
E is for Evolving: The mole is changing in size, shape, or color.
We provide leading-edge skin cancer treatment (in Bangalore) with the highest quality of care.
Several risk factors make a person more likely to get basal cell or squamous cell skin cancer.
Ultraviolet (UV) light exposure: Exposure to ultraviolet (UV) rays is thought to be the major risk factor for most skin cancers. Sunlight is the main source of UV rays. Tanning beds are another source of UV rays.
Having light-colored skin: Anyone can get skin cancer, but people with light-colored skin have a much higher risk than people with naturally darker skin color.
Being older: The risk of getting basal and squamous cell skin cancers rises as people get older. This is probably because of the buildup of sun exposure over time. But these cancers are becoming more common in younger people as well, probably because they are spending more time in the sun with their skin exposed.
Exposure to certain chemicals: Being exposed to large amounts of arsenic increases the risk of developing skin cancer. Arsenic is an element found naturally in well water in some areas. It's also used in making some pesticides and in some other industries.
Radiation exposure: People who have had radiation treatment have a higher risk of developing skin cancer in the area that received the treatment.
Long-term or severe skin inflammation or injury: Scars from severe burns, areas of skin over serious bone infections, and skin damaged by some severe inflammatory skin diseases are more likely to develop skin cancers, although this risk is generally small.
Psoriasis treatment: Psoralens and ultraviolet light (PUVA) treatments given to some patients with psoriasis (a chronic inflammatory skin disease) can increase the risk of developing squamous cell skin cancer and probably other skin cancers.
Xeroderma pigmentosum (XP): This very rare inherited condition reduces the ability of skin cells to repair DNA damage caused by sun exposure. People with this disorder often develop many skin cancers, starting in childhood.
Weakened immune system: The immune system helps the body fight cancers of the skin and other organs. People with weakened immune systems (from certain diseases or medical treatments) are more likely to develop many types of skin cancer.
Basal and squamous cell skin cancers are the most common types of skin cancer. They start in the top layer of skin (the epidermis), and are often related to sun exposure. Most skin cancers start in the top layer of skin, called the epidermis. There are 3 main types of cells in this layer:
Squamous cells: These are flat cells in the upper (outer) part of the epidermis, which are constantly shed as new ones form. When these cells grow out of control, they can develop into squamous cell skin cancer (also called squamous cell carcinoma).
Basal cells: These cells are in the lower part of the epidermis, called the basal cell layer. These cells constantly divide to form new cells to replace the squamous cells that wear off the skin's surface. As these cells move up in the epidermis, they get flatter, eventually becoming squamous cells. Skin cancers that start in the basal cell layer are called basal cell skin cancers or basal cell carcinomas.
Melanocytes: These cells make the brown pigment called melanin, which gives the skin its tan or brown color. Melanin acts as the body's natural sunscreen, protecting the deeper layers of the skin from some of the harmful effects of the sun. Melanoma skin cancer starts in these cells.
Basal cell carcinoma: (also called basal cell skin cancer) is most common type of skin cancer. These cancers start in the basal cell layer, which is the lower part of the epidermis. These cancers usually develop on sun-exposed areas, especially the face, head, and neck. They tend to grow slowly. It's very rare for a basal cell cancer to spread to other parts of the body. But if it's left untreated, basal cell cancer can grow into nearby areas and invade the bone or other tissues beneath the skin. If not removed completely, basal cell carcinoma can come back (recur) in the same place on the skin. People who have had basal cell skin cancers are also more likely to get new ones in other places.
Squamous cell carcinoma: These cancers start in the flat cells in the upper (outer) part of the epidermis. These cancers commonly appear on sun-exposed areas of the body such as the face, ears, neck, lips, and backs of the hands. They can also develop in scars or chronic skin sores elsewhere. They sometimes start in actinic keratoses. Less often, they form in the skin of the genital area. Squamous cell cancers can usually be removed completely (or treated in other ways), although they are more likely than basal cell cancers to grow into deeper layers of skin and spread to other parts of the body.
Other types of skin cancer: Melanoma: These cancers develop from melanocytes, the pigment-making cells found in the epidermis. Melanomas are much less common than basal and squamous cell cancers, but they are more likely to grow and spread if left untreated.
Less common types of skin cancer: Other types of skin cancer are much less common and are treated differently. These include:
1. Merkel cell carcinoma
2. Kaposi sarcoma
3. Cutaneous (skin) lymphoma
4. Skin adnexal tumors (tumors that start in hair follicles or skin glands)
5. Various types of sarcomas
Diagnosing skin cancer usually begins with a visual examination. You may be referred to undergo more specialized tests and make a diagnosis.
Skin biopsy: If the doctor thinks a spot might be a melanoma, the suspicious area will be removed and sent to a lab to be looked at under a microscope. This is called a skin biopsy.
Imaging tests: Imaging tests use x-rays, magnetic fields, or radioactive substances to create pictures of the inside of the body. They are used mainly to look for the possible spread of melanoma to lymph nodes or other organs. These tests are not needed for most people with very early-stage melanoma, which is very unlikely to have spread. Ultrasound, Computed tomography (CT) scan, Magnetic resonance imaging (MRI) scan, Positron emission tomography (PET) scan are also used for diagnosis of skin cancer.
We at CAN-C in Bangalore are committed to delivering the highest standard of treatment for skin cancer.
The stage is based on the results of the physical exam, the skin biopsy (and any other biopsies), and the results of imaging tests if they are done. Determining the stage of basal cell skin cancers is rarely needed, because these cancers are almost always cured before they spread to other parts of the body.
Squamous cell skin cancers are more likely to spread (although this risk is still small), so determining the stage can be more important, particularly in people who are at higher risk. Most squamous cell skin cancers occur in the head and neck region and tend to have a higher risk of recurring (coming back) or spreading compared to those in other locations.
How is the stage determined?
The system most often used to stage basal and squamous cell skin cancers is the TNM system. The stage is based on 3 key pieces of information:
The size of the tumor (T) and if it has grown deeper into nearby structures or tissues, such as a bone
If the cancer has spread to nearby lymph nodes (N)
If the cancer has spread (metastasized) to distant parts of the body (M)
Numbers or letters after T, N, and M provide more details about each of these factors. Higher numbers mean the cancer is more advanced.
CAN-C: Best centre for offering a full range of skin cancer treatments in Bangalore.
You can minimize your risk of skin cancer if you follow the steps below:
Limit your exposure to the sun and stay in the shade, especially during midday hours.
Wear clothing that covers your arms and legs.
Wear a hat with a wide brim to shade your face, head, ears, and neck.
Wear sunglasses that wrap around and block both UVA and UVB rays.
Use sunscreen and lip balm with a sun protection factor (SPF), and both UVA and UVB (broad spectrum) protection.
Avoid indoor tanning.
Examine your skin once a month. Tell your health care professional about skin changes.
Don't burn! Sunburns, especially on children, have been linked to an increased risk of developing melanoma later in life.
"CAN-C: Expertise in skin cancer treatment in Bangalore."
Make An Appointment Today
How Skin Cancer is treated?
Most skin cancers are detected and cured before they spread. The choice of treatment will depend on the tumor type. Your skin cancer treatment includes a plan customized to your specific type of cancer. Basal and squamous cell skin cancers and melanoma cancers are usually removed by one or combination of the treatments listed below.
Surgery is a common treatment for basal cell and squamous cell skin cancers. Different surgical techniques can be used. The options depend on the type of skin cancer, how large the cancer is, where it is on the body, and other factors. For skin cancers with a high risk of spreading, surgery sometimes will be followed by other treatments, such as radiation or chemotherapy.
1. Excision: This is similar to an excisional biopsy, but in this case the diagnosis is already known. For this procedure, the skin is first numbed with a local anesthetic. The tumor is then cut out with a surgical knife, along with some surrounding normal skin. Most often, the remaining skin is then carefully stitched back together. This type of surgery will leave a scar.
2. Curettage and electrodesiccation: In this treatment, the doctor removes the cancer by scraping it with a long, thin instrument with a sharp looped edge on one end (called a curette). The area is then treated with an electric needle (electrode) to destroy any remaining cancer cells. Curettage and electrodesiccation is a good treatment for superficial (confined to the top layer of skin) basal cell and squamous cell cancers. It will leave a scar.
3. Mohs surgery: Mohs surgery (also known as Mohs micrographic surgery, or MMS) is sometimes used when there is a high risk the skin cancer will come back after treatment, when the extent of the skin cancer is not known, or when the goal is to save as much healthy skin as possible, such as with cancers near the eye or other critical areas such as the central part of the face, the ears, or fingers.
4. Lymph node surgery: If lymph nodes near a squamous or basal cell skin cancer are enlarged, the doctor might biopsy them to check for cancer cells.
5. Sometimes, many nodes might be removed in a more extensive operation called a lymph node dissection: The nodes are then looked at under a microscope for signs of cancer. This type of operation is more extensive than surgery.
6. Skin grafting and reconstructive surgery: After surgery to remove a large basal or squamous cell skin cancer, it may not be possible to stretch the nearby skin enough to stitch the edges of the wound together. In these cases, healthy skin can be taken from another part of the body and grafted over the wound to help it heal and to restore the appearance of the affected area. Other reconstructive surgical procedures, such as moving 'flaps' of nearby skin over the wound, can also be helpful in some cases.
Over the years, we have been specialized in the treatment of skin cancer in Bangalore.
For Basal cell and Squamous Cell Skin Cancer:
Radiation therapy uses high-energy rays (such as x-rays) or particles (such as photons, electrons, or protons) to kill cancer cells.
When is radiation therapy used?
If a tumor is very large or is on an area of the skin that makes it hard to remove with surgery, radiation therapy may be used as the main treatment. Radiation therapy can also be useful for some patients who, for other health reasons, can't have surgery. Radiation therapy can often cure small basal or squamous cell skin cancers and can delay the growth of more advanced cancers.
Radiation is also useful when combined with other treatments. For example, radiation can be used after surgery as an adjuvant (additional) treatment to kill any small areas of remaining cancer cells that may not have been visible during surgery. This lowers the risk of cancer coming back after surgery. Radiation may also be used to help treat skin cancer that has spread to lymph nodes or other organs.
When radiation therapy is used to treat skin cancers, the radiation is focused from outside the body onto the tumor. This is often done using a beam of low-energy x-rays (superficial radiation therapy) or electrons (electron beam radiation). These types of radiation don't go any deeper than the skin. This helps limit the side effects to other organs and body tissues.
Getting radiation treatment is much like getting an x-ray, but the radiation is stronger and aimed more precisely at the cancer. The procedure itself is painless.
For Melanoma Skin Cancer:
When might radiation therapy be used?
1. Radiation therapy is not needed for most people with melanoma on the skin, although it might be useful in certain situations
2. It might be an option to treat very early stage melanomas, if surgery can't be done for some reason.
3. Radiation can also be used after surgery for an uncommon type of melanoma known as desmoplastic melanoma.
4. Sometimes, radiation is given after surgery in the area where lymph nodes were removed, especially if many of the nodes contained cancer cells. This is to try to lower the chance that the cancer will come back.
5. Radiation can be used to treat melanoma that has come back after surgery, either in the skin or lymph nodes, or to help treat distant spread of the disease.
6. Radiation therapy is often used to relieve symptoms caused by the spread of the melanoma, especially to the brain or bones. Treatment with the goal of relieving symptoms is called palliative therapy. Palliative radiation therapy is not expected to cure the cancer, but it might help shrink it or slow its growth for a time to help control some of the symptoms.
For Merkel Skin Cancer:
When might radiation therapy be used?
1. To treat the area of the main (primary) skin tumor after surgery to try to kill any cancer cells that might have been left behind. (You may hear this called adjuvant radiation.) This is especially important if there's a high chance that the cancer will come back (such as if the main tumor was large).
2. To treat the main tumor if surgery isn't an option, such as if a person isn't healthy enough for surgery or the tumor is in a place where all of it can't be removed.
3. To treat the lymph nodes near the main tumor. If a sentinel lymph node biopsy (or other type of biopsy) found cancer in the lymph nodes, if the results of the biopsy were not clear, or if a biopsy wasn't done, radiation therapy is often given to the lymph nodes in the area. This might be done after a lymph node dissection, or it might even be done instead of a lymph node dissection.
4. To help treat MCC that has come back (recurred) after surgery, either in the skin or lymph nodes.
5. To help treat MCC that has spread to distant parts of the body, often along with other treatments. In this case, the radiation is used to help shrink or slow the growth of the cancer and/or to help ease symptoms caused by its spread, but it's not expected to cure the cancer.
Chemotherapy (chemo) uses anti-cancer drugs that kill cancer cells. The drugs are usually injected into a vein or taken by mouth as a pill. They travel through the bloodstream to all parts of the body and attack cancer cells that have already spread beyond the skin.
Systemic Chemotherapy for Basal and Squamous Cell Skin Cancer:
Systemic chemotherapy (chemo) uses anti-cancer drugs that are injected into a vein or given by mouth. These drugs travel through the bloodstream to all parts of the body. Unlike topical chemotherapy, which is applied to the skin, systemic chemotherapy can attack cancer cells that have spread to lymph nodes and other organs.
If squamous cell carcinoma has spread, chemo might be an option, although an immunotherapy drug might be used first.
If chemo is used, drugs such as cisplatin and 5-fluorouracil (5-FU) might be options. These drugs are given into a vein (intravenously, or IV). They can often slow the spread of these cancers and relieve some symptoms. In some cases, they might shrink tumors enough so that other treatments such as surgery or radiation therapy can be used.
Melanoma Skin Cancer:
Chemo might be used to treat advanced melanoma after other treatments have been tried, but it's not often used as the first treatment because newer forms of immunotherapy and targeted drugs are typically more effective. Chemo is usually not as helpful for melanoma as it is for some other types of cancer, but it can shrink tumors in some people.
Several chemo drugs can be used to treat melanoma: Dacarbazine (also called DTIC), Temozolomide,
Nab-paclitaxel, Paclitaxel, Cisplatin, Carboplatin
Merkel Skin Cancer:
Chemo is most likely to be helpful for MCC that has spread to other organs. So far it's not clear if it can be helpful for cancers that are still just in the skin or that have only spread to nearby lymph nodes.
Merkel cell carcinoma (MCC) is rare, so it's been hard to study the use of chemotherapy for MCC in clinical trials. Because of this, doctors often use chemo drugs that have been helpful in treating other types of fast-growing neuroendocrine tumors. The most commonly used drugs for MCCs that have spread include: Cisplatin, Carboplatin, Etoposide, Topotecan
CAN-C: Leading cancer centre for skin cancer treatment in Bangalore.
Targeted Therapy for Basal and Squamous Cell Skin Cancer:
These drugs target parts of skin cancer cells that make them different from normal skin cells. Targeted drugs work differently from standard chemotherapy drugs. They may work sometimes when chemotherapy drugs don't.
Hedgehog pathway inhibitors: Vismodegib (Erivedge) and sonidegib (Odomzo) are targeted drugs that can be used to treat some advanced or recurrent basal cell skin cancers.
EGFR inhibitors: Squamous cell skin cancer cells often have too much of a protein called EGFR on their surfaces, which can help them grow. Drugs that target this protein, such cetuximab (Erbitux), have been shown to shrink some of these cancers.
Melanoma Skin Cancer:
These drugs target parts of melanoma cells that make them different from normal cells. Targeted drugs work differently from standard chemotherapy drugs, which basically attack any quickly dividing cells.
Targeted drugs can be very helpful in treating melanomas that have certain gene changes.
1. Drugs that target cells with BRAF gene changes: About half of all melanomas have changes (mutations) in the BRAF gene. Melanoma cells with these changes make an altered BRAF protein that helps them grow. Some drugs target this and related proteins, such as the MEK proteins.
Most often, if a person has a BRAF mutation and needs targeted therapy, they will get both a BRAF inhibitor and a MEK inhibitor, as combining these drugs often works better than either one alone.
BRAF inhibitors: Vemurafenib (Zelboraf), dabrafenib (Tafinlar), and encorafenib (Braftovi) are drugs that attack the BRAF protein directly.
MEK inhibitors: The MEK gene works together with the BRAF gene, so drugs that block MEK proteins can also help treat melanomas with BRAF gene changes. MEK inhibitors include trametinib (Mekinist), cobimetinib (Cotellic), and binimetinib (Mektovi).
2. Drugs that target cells with C-KIT gene changes: A small portion of melanomas have changes in the C-KIT gene that help them grow. These changes are more common in melanomas that start in certain parts of the body: On the palms of the hands, soles of the feet, or under the nails (known as acral melanomas), Inside the mouth or other mucosal (wet) areas, In areas that get chronic sun exposure.
Some targeted drugs, such as imatinib (Gleevec) and nilotinib (Tasigna), can affect cells with changes in C-KIT. If you have an advanced melanoma that started in one of these places, your doctor may test your melanoma cells for changes in the C-KIT gene, which might mean that one of these drugs could be helpful.
For Squamous Cell Skin Cancer:
The immune system normally helps protect the body against germs, and it can also help destroy cancer cells. Immunotherapy is the use of medicines to stimulate a person's own immune system to recognize and destroy cancer cells more effectively. It can be used to treat some people with advanced squamous cell skin cancer.
Immune checkpoint inhibitors: An important part of the immune system is its ability to keep itself from attacking normal cells. To do this, it uses "checkpoints", which are proteins on immune cells that need to be turned on (or off) to start an immune response.
Cancer cells sometimes use these checkpoints to avoid being attacked by the immune system. But drugs that target checkpoint proteins, called checkpoint inhibitors, can help restore the immune response against cancer cells.
Cemiplimab (Libtayo): Cemiplimab (Libtayo) is a drug that targets PD-1, a checkpoint protein on T cells (a type of immune system cell) that normally helps keep these cells from attacking other cells in the body. By blocking PD-1, this drug boosts the immune response against cancer cells.
Melanoma Skin Cancer:
Immunotherapy is the use of medicines to stimulate a person's own immune system to recognize and destroy cancer cells more effectively. Several types of immunotherapy can be used to treat melanoma.
1. Immune checkpoint inhibitors: An important part of the immune system is its ability to keep itself from attacking normal cells in the body. To do this, it uses "checkpoints," which are proteins on immune cells that need to be turned on (or off) to start an immune response. Melanoma cells sometimes use these checkpoints to avoid being attacked by the immune system. But these drugs target the checkpoint proteins, helping to restore the immune response against melanoma cells.
PD-1 inhibitors: Pembrolizumab (Keytruda) and nivolumab (Opdivo) are drugs that target PD-1, a protein on immune system cells called T cells that normally help keep these cells from attacking other cells in the body. By blocking PD-1, these drugs boost the immune response against melanoma cells. This can often shrink tumors and help people live longer.
CTLA-4 inhibitor: Ipilimumab (Yervoy) is another drug that boosts the immune response, but it has a different target. It blocks CTLA-4, another protein on T cells that normally helps keep them in check.
2. Interleukin-2 (IL-2): Interleukins are proteins in the body that boost the immune system in a general way. Man-made versions of interleukin-2 (IL-2) are sometimes used to treat melanoma. They are given as intravenous (IV) infusions, at least at first.
3.Oncolytic virus therapy: Viruses are a type of germ that can infect and kill cells. Some viruses can be altered in the lab so that they infect and kill mainly cancer cells. These are known as oncolytic viruses. Along with killing the cells directly, the viruses can also alert the immune system to attack the cancer cells.
4.Bacille Calmette-Guerin (BCG) vaccine: BCG is a germ related to the one that causes tuberculosis. BCG doesn't cause serious disease in humans, but it does activate the immune system.
5.Imiquimod cream: Imiquimod (Zyclara) is a drug that is put on the skin as a cream. It stimulates a local immune response against skin cancer cells.
For Merkel Cell Carcinoma:
Immunotherapy is the use of medicines that help a person's own immune system find and destroy cancer cells. This is a promising new form of treatment for Merkel cell carcinoma (MCC), especially if it has spread to other parts of the body.
Immune checkpoint inhibitors: An important part of the immune system is its ability to keep itself from attacking normal cells in the body. To do this, it uses "checkpoints." These are proteins on immune cells that need to be turned on (or off) to start an immune response. Cancer cells sometimes use these checkpoints to keep the immune system from attacking them.
Drugs that block either PD-1 or PD-L1 can stop this binding and boost the immune response against cancer cells. Examples of such drugs include: Avelumab (Bavencio®), which targets PD-L1, Pembrolizumab (Keytruda®) and nivolumab (Opdivo®), which block PD-1.
With our dedicated skin cancer specialist, we are able to deliver the highest quality skin cancer treatment (in Bangalore).
Our Doctors
Dr. Dinesh M G
Specialty: Surgical Oncologist & Laparoscopic Oncosurgeon
Dr. Dinesh M G, is an efficient surgeon specialized in oncology committed to the care and improvement of quality of life of cancer patients. His exceptional surgical skills, teamwork and knowledge are laudable. He is skilled in performing various minimal access oncologic surgeries and has mastered complex open surgeries in the field of oncology.
Completing MBBS from KIMS, Bangalore followed by MS - General Surgery from JJM Medical College, Davangere and M. Ch - Surgical Oncology from Kidwai Memorial Institute of Oncology, he has a Fellowship in Minimal Access Oncology from Basavatarakam Indo American Cancer Institute.

